
Contact Us

Stroke and brain lesions can significantly impair motor control, sensory processing, speech, memory, and emotional regulation.
At Neurotherapeutix in New York City, we offer non-invasive, image-guided TMS therapy to support neurological recovery and help restore lost function.
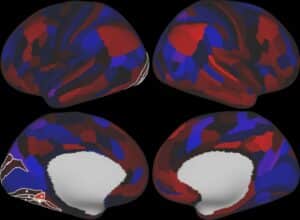
Using resting-state functional MRI (rsfMRI) to identify brain network disruptions, our fMRI-guided TMS targets the regions most impacted by stroke or brain injury.
This personalized approach promotes neuroplasticity and helps reestablish communication between brain regions.
If you’re seeking innovative stroke treatment or brain lesion therapy in NYC, we’re here to help. Continue reading or contact us directly to learn more.
A stroke occurs when blood flow to a part of the brain is interrupted, causing cells to die.
Brain lesions refer to areas of damaged brain tissue caused by stroke, trauma, tumors, infection, or surgery.
Both stroke and brain lesions can result in long-term neurological challenges, including physical, cognitive, and emotional impairments.
People recovering from stroke or brain lesions may experience a wide range of symptoms, depending on the areas of the brain affected. These may include:
Several medical, environmental, and genetic factors can increase the risk of stroke or lead to brain lesions, including:
Damage from stroke or lesions can impair:
These effects may persist long after the initial injury, often requiring long-term rehabilitation.
At Neurotherapeutix, we use fMRI-guided TMS to stimulate the brain networks disrupted by stroke or brain injury.
This technique is used for a wide range of neurological conditions and promotes neuroplasticity, the brain’s ability to reorganize and form new connections, which supports motor and cognitive recovery.
Research has shown that repetitive TMS (rTMS) applied to the dorsolateral prefrontal cortex (DLPFC) and motor cortex can:
In clinical experience, TMS has effectively targeted both the ipsilesional (same side as the lesion) and contralesional (opposite side of the lesion) hemispheres, depending on the nature of the damage.
Transcranial magnetic stimulation (TMS) delivers focused magnetic pulses to underactive or disrupted brain regions.
In stroke recovery, TMS is often applied to the motor cortex or prefrontal cortex to promote neuroplasticity, the brain’s ability to reorganize and form new connections.
Guided by resting-state fMRI, our approach targets the exact neural circuits affected by stroke, helping to restore function in areas related to movement, speech, and cognition.
Brain lesions from trauma, tumors, surgery, or infection can interrupt communication between brain regions.
TMS therapy helps re-engage these disconnected networks by stimulating healthy areas to compensate for damaged ones.
Using fMRI-guided precision, we tailor each treatment to the individual’s brain connectivity patterns, improving cognitive function, emotional regulation, and sensory processing impacted by brain lesions.
At Neurotherapeutix, TMS therapy is integrated into comprehensive post-stroke rehabilitation to complement physical, occupational, and speech therapies.
By stimulating key brain regions responsible for motor and cognitive tasks, TMS enhances the effects of traditional rehab, often accelerating recovery timelines.
Our clients have experienced improvements in upper limb coordination, mood stabilization, and communication abilities, even months or years after their stroke.
Unlike standard rehabilitation alone, fMRI-guided TMS offers:
TMS can be integrated with physical, occupational, or speech therapy to amplify results.
Your recovery begins with a detailed clinical evaluation and brain scan. From there, our team will:
All sessions are outpatient, non-invasive, and designed for comfort and safety.
TMS may benefit individuals who:
We also work with patients experiencing brain lesion-related symptoms due to trauma, surgery, or other causes.
At Neurotherapeutix, we combine leading-edge imaging and neuromodulation to help patients reclaim function and quality of life after brain injury.
Our stroke and brain lesion recovery program is built on science, compassion, and personalized care.
Request an appointment or contact us today to begin your recovery journey with fMRI-guided TMS therapy.
Call us at (917) 388-3090 or click to request a regular or telehealth appointment.
Neurotherapeutix
171 East 74th Street, Unit 1-1 New York, NY 10021

Neurotherapeutix is the leading clinic for functional imaging guided transcranial magnetic stimulation (TMS), a safe, innovative, and non-invasive methodology for treating a wide range of acute and chronic mental disorders and brain injuries. Our advanced fMRI technology allows us to map the brain for the… Learn More »
By: Neurotherapeutix NYC
Reviewed By: Marta Moreno, Ph.D
Published: March 24, 2023
Last Reviewed: September 27, 2024
QUICK INQUIRY
Contact us to get an estimate for your medical services requirements. You can fill in the form to specify your medical requirements or you can call us directly.